Towards
the end of the year, you have guests from the Veterinary Health
Directorate, Ministry of Agriculture. This team will introduce zoonotic
diseases in Indonesia, including one material that makes me interested,
which is about rabies.
As
a child, I had seen one of the neighbors who was bitten by a dog.
Although in the end he was healthy again without any symptoms of
exposure to rabies, at that time we were aware of the disease due to
this dog bite.
Not
to mention some time ago having a video show showing the condition of a
child after being bitten by a dog. Of the symptoms that subside when
given water, it can be ascertained that more than 90% cannot be saved.
It is sad, but rabies education as part of zoonotic disease has not
been understood by many people.
Thank God the material provided by the source really opened up our insight into zoonosis. In addition to COVID-19 and rabies, it turns out that there are still many other zoonotic diseases. Anything, huh?
Avian Influenza/bird flu
Bird
flu was known to the Indonesian people at the end of 2003 when a lot of
poultry (chicken and birds) died suddenly. In Indonesia, avian
influenza was discovered in late 2003. The case was last reported in
2017.
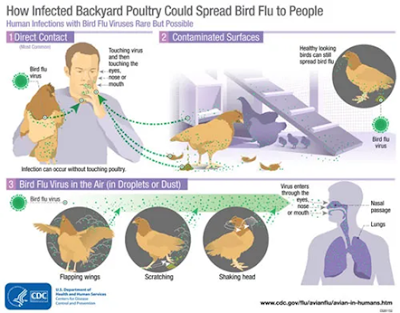
Bird
flu viruses spread through saliva, mucus, and poultry droppings and are transmitted to humans through one’s eyes, nose, or mouth, or inhaled.
Clinical symptoms in humans can be fever, cough, sore throat, muscle
aches, headaches, runny nose, clogged nose, respiratory
failure, pneumonia, or damage to the organs of the body.
Prevention
of bird flu can be done by vaccinating poultry (birds or chickens) and
preventing the transmission of bird flu to humans by maintaining
cleanliness when raising poultry, including buying poultry meat in
markets whose cleanliness is well maintained.
The
source also explained how to cook chicken and egg meat with temperatures
reaching > 70°C. Since I’m very happy with half-baked eggs, I must
start to avoid my hobby.
Anthrax
Menong's
friend must have remembered the case of the anthrax in the Kulon Progo
area, which was then electrifying. This case stems from people who
consume dead beef that has been buried. After being traced, there were
about 125 people who were sampled for blood due to consumption and contact
with cows that had been exposed to anthrax.
The
anthrax is caused by the bacteria Bacillus anthracis and inflammation
of the spleen (jawa) datau ceunang hideung (sunda). Hot-blooded animals
(cows, sheep, horses, and pigs), including humans, are prone to anthrax.
Generally,
animals are exposed to anthrax because they are infected by anthrax
bacterial spores that are in the soil or feed. Humans themselves can be
infected from direct contact of blisters or sores with anthrax spores
in soil or animals containing anthrax bacteria. Or breathing air exposed
to anthrax spores. Farmers, grass nurseries, ranchers, animal
slaughterers, and animal health workers are vulnerable to this spread.
This is why the area that has been infected with anthrax or the location where to bury anthrax animals must be marked so that no one has opened the land. Anthrax bacteria can survive in the soil for up to 200 years. This is what makes anthrax very dangerous for animals and humans.
Anthrax
is also spread through livestock meat products that are sick with
anthrax or livestock products such as jerky, skin crackers, and others
consumed by humans.
Leptospirosis
Leptospirosis
was caused by the urine of rats, and I began to know in the early 2000s
when there was a major flood in the Jakarta area. The incidence of
leptospirosis will experience a surge in the presence of floods due to
the flow of water contaminated with the urine of rats infected with
Leptospirosis bacteria.
Globally,
leptospirosis cases are estimated at 1 million cases, with the deaths
of 60,000 people. In Indonesia, leptospirosis events almost occur in all
provinces, especially most provinces in Java and Sumatra, Bali, West
Nusa Tenggara, South Sulawesi, North Sulawesi, East Kalimantan, and West
Kalimantan.
Leptospirosis gives symptoms in humans in the form of acute fever, urine bleeding, kidney failure, and death.
Brucellosis
I
just heard the term "disease caused by this brucella bacteria."
Brucellosis is a disease that is transmitted through the digestive
tract, genital tract, and mucosa, or injured skin. In general, human
transmission occurs through the consumption of immature milk or contact
with the secretion of infected animals.
The
intermediate animals of this disease are cows and goats and are caused
by poor sanitation. And (again), we are reminded to avoid the
consumption of raw milk and immature meat.
Brucellosis in animals and humans will cause abortion or miscarriage of the fetus.
Education
about zoonotic disease in Indonesia is very necessary so that there are
no more victims of children or adults who suffer from dogs or residents
who do not understand the determination to eat meat that turns out to
be affected by anthrax.





Post a Comment
Post a Comment